
INTRODUCTION
HQP1351 (olverembatinib) is an orally active third-generation BCR-ABL TKI designed for treatment of the patients with CML, harboring T315I mutation, which confers resistance against all first- and second-generation TKIs.
METHODS
The TKI resistant CML patients harboring T315I mutations either in chronic-phase (CP), or in accelerated-phase (AP), were enrolled into two single-arm, multicenter, open-label pivotal studies: HQP1351-CC201 in and HQP1351-CC202, respectively. The HQP1351 was administered at 40 mg once every other day (QOD) for 28 consecutive days per cycle over 24 months. The primary objective was to evaluate efficacy by major cytogenetic response (MCyR) in patients with CML-CP and major hematologic response (MaHR) in CML-AP. Secondary objectives included safety, tolerability, and pharmacokinetics (PK).
RESULTS
Baseline characteristics
Study CC201 (CML-CP)
As of the study cut-off date of March 23, 2020, total 41 patients were enrolled, of whom 38 (92.7%) completed ≥ 6 cycles and 21 (51.2%) were male. Median (range) follow-up was 7.9 (3.1-11.1) months, median age was 47 (22-70) years old. Median (range) interval from CML diagnosis to first HQP1351 treatment was 5.31 (0.6-23.2) years, and 32 (78.1%) patients received ≥ 2 prior lines of TKI. Three patients withdrew from the study-due to progressive disease (PD), intolerance, or consent withdrawal.
Study CC202 (CML-AP)
As of the cut-off date of February 11, 2020, total 23 patients were enrolled, of whom 18 (78.3%) completed ≥ 6 cycles and 18 (78.3%) were male. Follow-up duration was 8.2 (1.4-9.6) months, median age was 41 (21-74) years old. Median interval from CML diagnosis to first dose of HQP1351 was 4.96 (0.4-10.2) years, and 18 (78.3%) patients received ≥ 2 prior TKIs. Five patients withdrew because of PD or intolerance before Cycle 6.
Efficacy
Study CC201 (CML-CP)
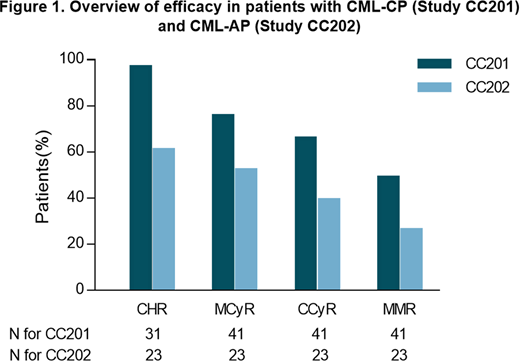
Across a median follow-up of 7.9 months, the mean (95% CI) 3-month progression-free survival (PFS) was 100% (100-100%) and 6-month PFS 96.7% (78.6-99.5%) because of 1 PD. In 31 evaluable patients who did not have a complete hematologic response (CHR) at baseline, 30 (96.8%) achieved CHR. In 41 evaluable patients who did not have a complete CyR (CCyR) at baseline, 31 (75.6%) achieved MCyR, including 27 (65.9%) CCyR and 4 (9.8%) partial CyR (PCyR). Total 20 out of 41 (48.8%) evaluable patients achieved major molecular response (MMR; Figure 1).
Study CC202 (CML-AP)
Across a median follow-up of 8.2 months, the 3-month PFS was 100% (100-100%) and the 6- month PFS 95.5% (71.9-99.3%) because of 2 PDs. A total of 18 (78.3%) of 23 evaluable patients without MaHR at baseline achieved MaHR, including 14 (60.9%) with CHR. In the 23 evaluable patients without MCyR at baseline, 12 (52.2%) patients achieved MCyR, including 9 (39.1%) CCyR and 3 (13.1%) PCyR. A total of 6 out of 23 (26.1%) evaluable patients achieved MMR (Figure 1).
HQP1351 was highly and durably efficacious in the CML patients with T315I mutation; the probability and depth of clinical response may increase with prolonged treatment period.
Safety/tolerability
Study CC201
Frequent treatment-related adverse events (TRAEs; all grades; G3-4) included thrombocytopenia (65.9%; 48.8%), followed by anemia (48.8%; 24.4%), leukopenia (46.3%; 12.2%), and neutropenia (36.6%; 19.5%). Common non-hematologic TRAEs of any grade included skin pigmentation (53.7%) as well as elevations in creatine kinase (48.8%), ALT (31.7%) and AST (26.8% which most were grade 1 - 2. No death occurred.
Study CC202
Common TRAEs (all grades; G3-4; serious AE [SAE]) included thrombocytopenia (73.9%; 52.2%; 17.4%), anemia (65.2%; 39.1%; 13.0%), leukopenia (56.5%; 30.4%; 0%), and neutropenia (26.1%; 21.7%; 0%;). Common non-hematologic AEs included skin pigmentation (69.6%), hypocalcemia (52.2%), proteinuria (52.2%), hypertriglyceridemia (47.8%), hyperphosphatemia (43.5%), arthralgia (34.8%), and fatigue (26.1%), of which most were grade 1- 2.
CONCLUSIONS
HQP1351 has been shown highly efficacious in heavily TKI-pretreated patients with T315I-mutated CML-CP or CML-AP and was well tolerated. Registration: Clinicaltrials.gov identifier NCT03883087 (Study HQP1351-CC201) NCT03883100 (Study HQP1351-CC202).
Chen:Ascentage Pharma Group: Current Employment. Niu:Ascentage Pharma Group: Current Employment. Zeng:Ascentage Pharma Group: Current Employment. Men:Ascentage Pharma Group: Current Employment. Lu:Ascentage Pharma Group: Current Employment, Current equity holder in publicly-traded company. Wang:Ascentage Pharma Group: Current Employment. JI:Ascentage Pharma Group: Current Employment. Yue:Ascentage Pharma Group: Current Employment. Yang:Ascentage Pharma (SuZhou) Co., Ltd: Current Employment, Current equity holder in publicly-traded company, Other: Leadership and other ownership interests. Zhai:Ascentage Pharma (SuZhou) Co., Ltd: Current Employment, Current equity holder in publicly-traded company, Other: Leadership and other ownership interests.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal